"You tell me what you need people to do, and I’ll tell you how to help them do it.” Although a simplification, this statement by social and behavioral scientists to our infectious disease colleagues illustrates the nature of our collaboration during an infectious disease outbreak like the current COVID-19 outbreak. Without this collaboration, we risk that people will not do what we are telling them to do.
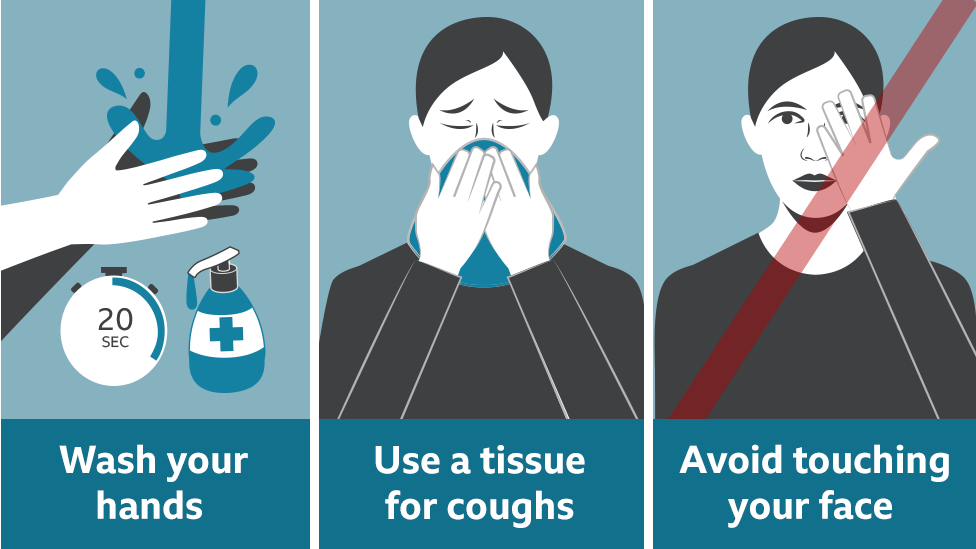
That’s because telling people what to do is often a necessary but seldom a sufficient condition for them to do it. In response to COVID-19, the CDC’s recommendations for preventing infection and disease spread are as follows:
- Avoid close contact with those who are sick
- Stay home when you are sick, except to get medical care
- Cover your coughs and sneezes with a tissue
- Clean frequently touched surfaces and objects daily using regular household detergent and water
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating, and after blowing your nose, coughing, or sneezing
Others have written recently about how behavior change principles can be used to encourage people to engage in these behaviors (see Michie and Hallsworth). For this blog, I will highlight some of the recent research on how to encourage people to wash their hands and stay home from work when sick.
Handwashing
Not surprisingly, much of the research on encouraging handwashing has occurred in healthcare settings. A recent Cochrane review of interventions to improve hand hygiene adherence in patient care settings found that a number of strategies, particularly in combination, increased handwashing behavior. In addition to education, placing handwashing and hand-sanitizing facilities near patient care areas, providing regular cues or reminders to wash, and providing performance feedback improved handwashing compliance. For example, a study of this combination intervention approach in rural hospitals showed a 20% improvement in intervention hospitals vs. a 3% decrease in control hospitals for handwashing adherence.
There is less research on how to promote handwashing in community and home settings. A recent review of handwashing promotion interventions targeting children in low- and middle-income countries concluded that there is a paucity of evidence on how to encourage handwashing. Some recent studies, however, have shown promising results. For example, a study in Bangladesh primary schools using behavioral “nudges” (environmental changes to make handwashing more convenient) increased handwashing from 4% to 74% following latrine use. In aggregate, the research on promoting handwashing shows that, in addition to education, providing greater access to handwashing facilities, particularly in low income areas with inadequate access, as well as regular reminders and feedback, increases handwashing behavior.
Staying home from work when sick
You might think that telling people to stay home from work when they are sick should be enough for them to comply, but it is not. A study of Belgium workers showed that 62% went to work while sick, including both infectious and non-infectious sickness. A recent study in Australia compared laboratory-confirmed influenza cases with history of sick leave among healthcare workers and found that 14% worked while sick with the flu. A review of studies on influenza transmission in the workplace found expected adherence with sick leave recommendations ranged from 71 to 95 percent. Among the findings of these studies is that having supervisors supportive of taking sick leave when sick is beneficial, but only for those with paid sick leave.
Numerous studies have shown that workers with paid sick leave are more likely than those without this benefit to stay home when sick. For instance, a recent study using data from the Medical Expenditure Panel Survey found a 42% higher likelihood of staying home when sick with the flu among those with paid sick leave versus those without. A modeling simulation of a local flu outbreak showed that if paid sick leave was available to all employees, then workplace infection rates would decrease by nearly 6%, and that giving temporary “flu days” during an outbreak would decrease workplace infection rates by 25 to 39%. Not surprisingly, those without paid sick leave tend to be temporary or hourly workers. The modeling study above suggests that even a small temporary sick leave benefit for these employees during the COVID-19 outbreak could increase staying home when sick and reduce workplace transmission. When a vaccine to prevent COVID-19 eventually becomes available, paid sick leave also could increase vaccination rates. A survey during the H1N1 flu outbreak showed that those with paid sick leave were 30% more likely to be vaccinated for the flu.
A large body of research provides guidance on how to help people do what we need them to do to reduce the risk of infectious disease transmission. That research shows that we need to do more than educate people in what they need to do. We also need to remove barriers and provide incentives to adhere to these recommendations, particularly among those who suffer from considerable health inequities and could most benefit from greater access to handwashing facilities and to paid sick leave during the COVID-19 epidemic.