When the COVID-19 pandemic became widespread in the United States, much of the discussion and attention centered on urban epicenters with rapid spread due to the high population density. While rural areas are less populous, other characteristics of rural America make those individuals living there far more vulnerable than their urban counterparts. In this post we describe the unique dynamics making rural residents more vulnerable, provide a comparison of COVID-19 trends in rural and urban areas in Pennsylvania, and offer insight as to why the COVID-19 pandemic highlights and magnifies the longstanding factors contributing to rural-urban health disparities.
The Increased Vulnerability of Rural Residents
Chronic conditions
Individuals with pre-existing health conditions are considered among the highest at-risk for developing severe COVID-19 complications including those with chronic conditions, such as heart disease, respiratory diseases, lung cancer, and diabetes. Compared to their urban counterparts, rural America has a higher prevalence of these chronic health conditions, placing them at higher risk.
Age
COVID-19 is also more deadly for older adults, particularly those 65 and older. Rural counties have notably higher percentages of older residents than their urban counterparts – 21% of the urban population is 60 years or older compared to 26% of rural populations. This larger percentage of older adults in rural areas is not only problematic due to health concerns among the elderly, but also because of the potential spread of COVID-19 in assisted and long-term care facilities.
Race, ethnicity, and poverty
Another component to consider when examining the vulnerability of rural populations is the concentration of poverty in “rural ghettos” and the double jeopardy among rural people of color. Poverty rates are higher in non-metro areas regardless of race/ethnicity, but highest rates are experienced by rural individuals of color when compared to both rural whites and their urban racial/ethnic peers. That is, there is a compound penalty to being both a person of color and living outside of an urban location. Previous research suggests disproportionate premature mortality rates in rural counties, especially among non-Hispanic Black and American Indian populations, even pre COVID-19. These same groups are disproportionately impacted by COVID-19 across the U.S. Thus, there is reason to be concerned that residing in a rural location may amplify the impacts of and relationships between poverty, systemic racism in healthcare, COVID-19, and health comorbidities.
Correctional facilities
Rural communities have also been viewed as favorable locales for America’s prisons from the perspective of generating economic growth. Due to shared living quarters, overcrowding, and constant circulation of employees and inmates, controlling the spread of COVID-19 in correctional facilities is challenging. Most state correctional facilities in Pennsylvania are located in rural counties. In the case of Huntingdon County, the vast majority of COVID-19 cases were due to positive inmates or employees. Outbreaks within such institutions could quickly overburden the healthcare infrastructure of both prisons themselves and the rural communities in which they are found.
Healthcare infrastructure
Finally, rural areas are not necessarily equipped with the proper healthcare infrastructure necessary to handle any increase in rates of COVID-19. Since the mid-2000s, rural hospital closures have continued to rise due to lack of workforce, finances, and low occupancy. This, partnered with the lack of equipment and healthcare personnel at hospitals still in operation, greatly impacts the quality of and access to healthcare for rural residents.
Rural-Urban Pennsylvania Comparisons
To fully appreciate the unique circumstances faced in rural areas, we found it important to compare the impact of COVID-19 on rural and urban areas in Pennsylvania.
Using data published by the Pennsylvania Department of Health, we examined monthly county-level case rates from March 2020 to March 2021. In March 2020, the average case rate in the state was 20.7 cases per 100,000 individuals, without much variation among rural and urban counties. By September 30, the average had risen to 809.7 cases per 100,000. Delaware and Philadelphia counties topped the list with case rates of over 2,000 (per 100,000) each, while a number of counties along the Pennsylvania-New York border (Tioga, Cameron, Venango, McKean, Warren) had reported case rates of less than 200 each.
As previously explained, many characteristics of rural areas and their residents are cause for concern during health crises such as the COVID-19 pandemic. Using the classifications provided by the Center for Rural Pennsylvania, Figure 1 demonstrates the difference in average case rates for rural counties, urban counties, and the state as a whole. As of September 2020, the impact of COVID-19 on rural Pennsylvania had yet to be deeply experienced, as rural county case and death rate averages were still far below those of urban counties. At this time, the 19 urban counties of Pennsylvania reported an average case rate of 1,324.6, while rural counties had an average of 605.9 cases per 100,000 individuals.
Figure 1. Pennsylvania COVID-19 Case Averages
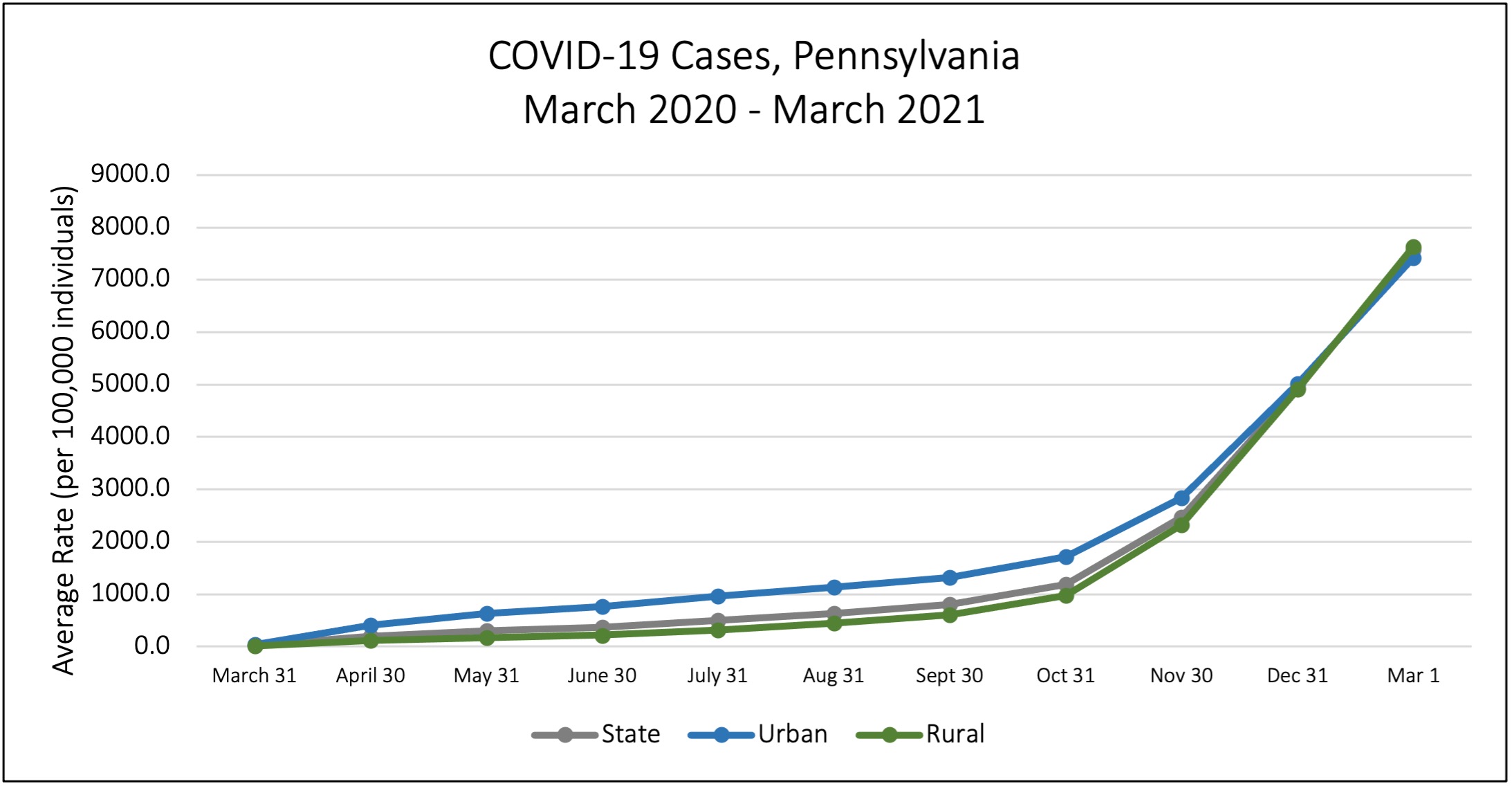
However, the spread of COVID-19 in the fall greatly impacted rural Pennsylvania. Both October and November demonstrate the rates beginning to converge. By December 31, 2020, the average case rate difference between rural and urban counties was indistinguishable. Urban counties average case rate was 5,014.6, while rural counties average case rate was 4,910.9 per 100,000 – a 0.1% difference in case rates. Currently, as of March 2021 rural county average case rates surpassed those of urban counties, 7635.7 per 100,000 and 7425.8 per 100,000 respectively.
Using the same rural-urban classifications, Figure 2 provides a look at the counties with the highest case rates per 100,000 as of September 30, 2020, December 31, 2020 and March 1, 2021. In September, only five rural counties (rural counties are in bold) were present among the 20 counties with the highest case rates in the Commonwealth. Columbia, Northumberland, and Monroe counties are all adjacent to urban counties that also make the top 20 list, mostly in and around the Scranton-Wilkes Barre area. These rural counties likely had high exposure from neighboring, more urbanized areas. By December 31, rural counties made up 15 of the 20 counties with the highest COVID-19 case rates. Most of these counties are either in Central Pennsylvania or along the Pennsylvania-West Virginia border. Almost a year into the COVID-19 pandemic, rural counties are still a heavy presence on this list, representing 14 of the top 20 counties. As of March 2021 we saw the addition of Forest and Lycoming, two counties that have not previously had such high average case rates. Forest County is one of Pennsylvania’s smallest counties with a population of 7,313; to date nearly 1 in 5 residents has tested positive for COVID-19 (18.9%).
Figure 2 . Pennsylvania Counties with Highest COVID-19 Case Rates
| County | 9/30/20 | County | 12/31/20 | County | 3/1/21 |
|---|---|---|---|---|---|
| Delaware | 2042.7 | Clearfield | 10399.6 | Forest | 18958.6 |
| Philadelphia | 2028.6 | Mifflin | 7394.7 | Clearfield | 16244.4 |
| Berks | 1710.3 | Huntingdon | 6796.8 | Union | 11753.9 |
| Centre | 1664.6 | Cambria | 6697.8 | Mifflin | 9921.7 |
| Lehigh | 1545.2 | Somerset | 6557.0 | Montour | 9753.3 |
| Northampton | 1483.9 | Union | 6455.3 | Huntingdon | 9316.3 |
| Montgomery | 1482.6 | Blair | 6438.0 | Lebanon | 9086.9 |
| Lancaster | 1470.5 | Montour | 6430.9 | Somerset | 9043.7 |
| Lebanon | 1470.5 | Lebanon | 6263.4 | Cambria | 8873.5 |
| Bucks | 1415.6 | Bedford | 6135.8 | Northampton | 8810.5 |
| Columbia | 1404.0 | Crawford | 5712.2 | Northumberland | 8760.1 |
| Dauphin | 1392.3 | Franklin | 5618.2 | Blair | 8665.9 |
| Chester | 1324.8 | Berks | 5578.7 | Berks | 8496.7 |
| Luzerne | 1301.8 | Philadelphia | 5564.5 | Schuylkill | 8476.3 |
| Lackawanna | 1230.6 | Fayette | 5555.8 | Lehigh | 8370.3 |
| Northumberland | 1171.5 | Lehigh | 5527.8 | Lycoming | 8195.2 |
| Beaver | 1167.9 | Westmoreland | 5514.1 | Franklin | 8086.0 |
| Franklin | 1159.3 | Centre | 5514.0 | Lancaster | 8040.6 |
| York | 1102.2 | Schuylkill | 5502.3 | Fayette | 8032.8 |
| Monroe | 1064.3 | Juniata | 5468.8 | York | 8003.6 |
Figure 3 highlights a similar pattern among death rates over the past year, as seen among average case rates. For all of 2020 urban counties had a higher death rate average, compared to rural counties. However, as of the beginning of 2021, rural counties transitioned to the top with a death rate average of 200.8 per 100,000, compared to 188 per 100,000 for urban counties.
Figure 3. Pennsylvania COVID-19 Death Averages
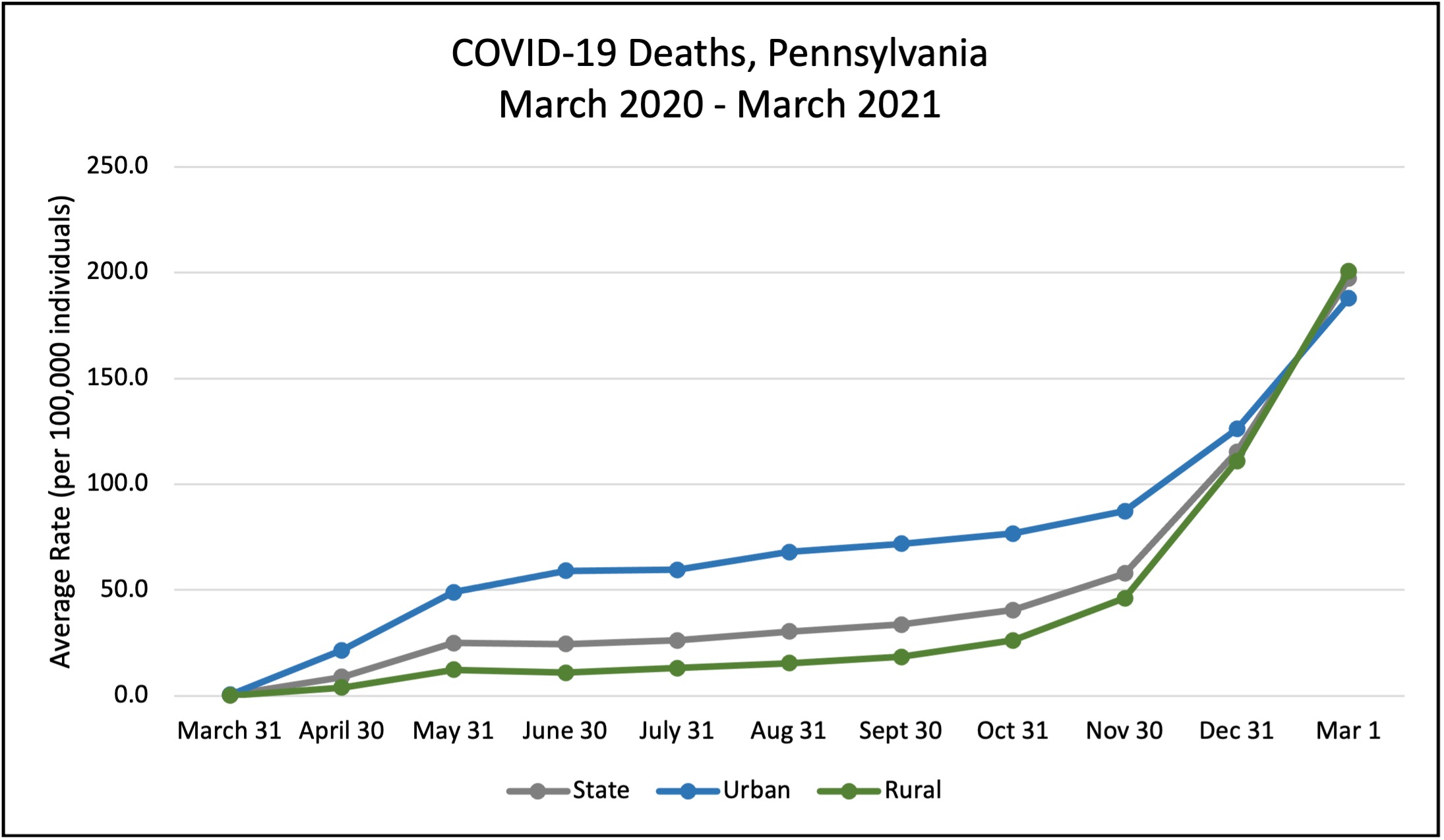
While population density appears to have played an important role early in the spread of COVID-19 at the county level in Pennsylvania, it did not continue to protect rural areas from infection. Rural areas and residents have many characteristics that make them high-risk. The lack of population density in these areas may have significantly contributed to the slower spread of the virus; however, the data demonstrate that population density may no longer have been a primary explanatory role by the beginning of 2021.
Looking ahead at vaccinations
As we move into the second year of the COVID-19 pandemic in the U.S. we are encountering new challenges to combatting the rural-urban divide. Rural communities face two major challenges with respect to vaccination and achieving herd immunity from widespread uptake: hesitancy and availability. Over a third (35%) of rural residents in the U.S. claim they will not or probably will not choose to obtain a COVID-19 vaccine, and almost two-thirds (62%) believe being vaccinated is a personal choice rather than a responsibility to protect others.
Conversely, those who may be interested in obtaining a vaccine may face unique obstacles inhibiting their access. In Pennsylvania specifically, the reliance on chain pharmacies for vaccine distribution, like RiteAid and CVS, leaves some rural residents with no access in their counties (Forest, Fulton, and Sullivan) or long transportation to the limited sites available in a county. Moreover, the reliance on internet for scheduling vaccination appointments may also be a larger burden for these individuals, as around 15% of rural households in PA may not have internet access. A number of rural counties are doing quite well with regard to vaccinations per 100,000, (including Adams, Clearfield, Cameron, and Sullivan) but this may also be explained by the heavy concentration of individuals employed in health and caring professions.
The COVID-19 pandemic has exacerbated problems that existed long before the emergence of this pandemic. Rural people and communities have been older, sicker, and experienced less access to healthcare for many years. However, in shedding light on this phenomenon, there is future promise. Addressing issues regarding poverty, availability and access to healthcare infrastructure, transportation, and internet access will assist in combatting not only COVID-19, but rural-urban health disparities in general.


